Periodic Limb Movement Disorder (PLMD): Treating Restless Limbs
Do your legs continually twitch when you’re in a movie theater or seated at dinner? Do random limb movements disrupt your slumber at night?
We’ve all heard of restless legs syndrome (RLS), but most patients don’t realize that restless limbs may point to a broader condition called periodic limb movement disorder (PLMD).
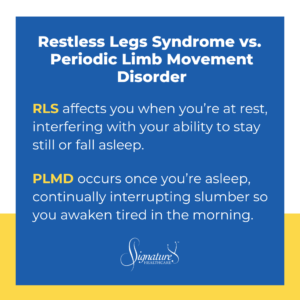
Here’s the difference:
- RLS affects you when you’re at rest, interfering with your ability to stay still or fall asleep.
- PLMD occurs once you’re asleep, continually interrupting slumber so you awaken tired in the morning.
People with periodic limb movement disorder frequently don’t know they have it. And PLMD is idiopathic, meaning medical science doesn’t completely understand why it happens.
About Restless Legs Syndrome (RLS)
With restless legs syndrome, the legs feel compelled to kick out or move around, typically when they’ve been at rest for a while. This can occur at bedtime or during the day.
Patients describe RLS in many ways, including:
- Crawling sensations
- Burning or tingling
- Jerkiness, tugging, or pulling
- Aching or soreness (not to be confused with leg cramps, a separate issue)
Standing, walking, or moving the legs back and forth in bed typically causes sensations to dissipate, but any of these symptoms can make it difficult to fall asleep.
RLS has undergone more study than the broader umbrella condition of PLMD. There are several theories about what causes restless legs, including a very strong hereditary component.
Sensations also occur more commonly as people age and, in my clinical experience, tend to affect women more than men.
About Periodic Limb Movement Disorder (PLMD)
Interestingly, most people with restless legs syndrome also have PLMD, while only about half of patients with PLMD have RLS.
While RLS alone can make it difficult to fall asleep, PLMD affects the patient’s sleep architecture — the critical sleep cycle itself. PLMD can include uncontrolled movement of both legs and arms, although it predominantly affects the lower extremities.
A patient with PLMD may get enough sleep, but the quality of their sleep suffers because of involuntary limb movements. Even after 10–12 hours of slumber, they wake up unrested and unrefreshed, similar to what people with sleep apnea report.
What Causes Involuntary Limb Movement?
Medical science is unclear on why periodic limb movement disrupts sleep architecture… and it may actually be the reverse.
Not everyone with restless legs is iron deficient, but a striking many are. When a patient reports involuntary movements, physicians typically check iron levels first. Iron deficiency from their monthly cycle may predispose some women to RLS and PLMD.
We also know that certain neurotransmitters and amino acids — dopamine, gamma-aminobutyric acid (GABA), endogenous endorphins, glutamine, glargine — are implicated as a cause of restless legs and likely play a role in PLMD, too.
But it’s unclear whether PLMD results from misfiring nerves in the brain because of one or more blocked neurotransmitters. Whatever the biochemical cause, a patient’s sleep becomes regularly and seriously disrupted.
Diagnosing Periodic Limb Movement Disorder
Two to three percent of the population is diagnosed with restless legs and/or PLMD.
If a patient suspects they have RLS, they likely also have PLMD. But because PLMD happens during sleep, many people may be relatively asymptomatic and unaware they have it.
If a patient comes to me complaining of restless legs symptoms and daytime fatigue — and they don’t have a weight or snoring issue — I usually treat them with medication to address the RLS, which may also correct PLMD, if present.
If that patient doesn’t have symptoms suggestive of RLS, if I’m unsure about the PLMD diagnosis, or if an initial trial of medication is not helpful, I suggest an in-lab sleep study to evaluate for PLMD.
What we find in the lab is often surprising: A patient may experience dozens of sleep arousals every hour, caused by periodic limb movement disorder.
With a diagnosis made, we can focus on treatment.
How Are RLS and PLMD Treated?
If we don’t pinpoint an underlying disease or condition, such as the aforementioned iron deficiency, we may choose to treat RLS and PLMD either via medication or a non-pharmacologic approach:
Non-Pharmacologic
A fairly new non-pharmacologic treatment for PLMD is via a neurostimulation device, similar to a TENS unit. The neurostimulator sends a constant, low-level signal from a patient’s calf and tibial nerve up the leg into the lumbosacral plexus in the lower back.
For some patients, the device eliminates leg restlessness, so they can nod off — and sleep undisturbed — with no medication.
Medication
Avoiding Reactions From Other Medications
For patients with restless legs, we typically consider any other prescriptions they take. For example, Benadryl — a sedating histamine blocker often used as a sleep medication — can also spur leg restlessness.
Some nausea medications and antidepressants may also contribute to restless limbs. If the prescribing doctor is made aware of the symptoms, those prescriptions can be adjusted accordingly.
Prescription Treatment
- Clonazepam: If a patient’s leg restlessness is occasionally bothersome (once or twice a month), we prescribe a low dose of clonazepam, a benzodiazepine that slows down the nervous system.
- Sinemet (carbidopa/levodopa): We also may prescribe Sinemet, a Parkinson’s disease treatment that combines carbidopa and levodopa to regulate low levels of dopamine in the brain.
For persistent cases of restlessness — that is, every two to three days to nightly onset — we may recommend regular prophylaxis with medications aimed at neurological disorders that affect movement control. These include:
Do Involuntary Movements Disturb Your Rest?
Uncontrolled or involuntary limb movement may stop you from getting to sleep or covertly disrupt sleep cycles after you nod off. Your Signature Healthcare physicians are here to help you achieve a healthy, restorative night’s rest.
We determine the core issue of your limb restlessness, address periodic limb movement disorder, and follow up to ensure you start your day healthy and energized.
Reach out today. Let’s get you a good night’s sleep.

Dr. Marshall Silverman
Dr. Marshall Silverman, MD, a board-certified internal medicine specialist with over two decades of experience in Charlotte, combines his clinical role with academic pursuits as a clinical associate professor at UNC-Chapel Hill. His diverse interests span from disc golfing and woodworking to playing the violin and authoring illustrated children’s poetry books, reflecting a unique blend of medical professionalism and creative expression.

