Myths Debunked and Interesting Facts About Menopause
Menopause is not an event. It’s a process that occurs naturally over a decade or so. A woman (average age is 51) is clinically diagnosed as menopausal when she hasn’t had a monthly period for 12 months.
The preliminary stage, known as perimenopause, can occur years before menopause and is often referred to as “reverse puberty.” The ovaries gradually shut down, and hormone levels start to change, which can lead to side effects.
Some women might not recognize perimenopause side effects if their menstrual periods haven’t changed. Others may experience uncomfortable perimenopausal symptoms in their 40s without a clear diagnosis or treatment. Their doctor may attribute these symptoms to a “midlife crisis,” stressful work commitments, or heavy family obligations.
Let’s address some myths and cover other interesting facts about menopause.
Menopause Myths
Menopause and perimenopause may seem intimidating or mysterious — and myths are commonplace.
Myth: You can’t get pregnant once you enter perimenopause or menopause.
Although rare, you can get pregnant. As a woman’s periods begin to change or diminish with age, conception is rare but not impossible. It’s important to continue using contraceptives for another year after your cycle slows down.
Myth: Approaching menopause means hot flashes.
Hot flashes can signal perimenopause. But they’re just one symptom, and not everyone gets them.
Hormonal changes during perimenopause and early menopause often depend on your genetics and lead to various symptoms beyond hot flashes, like:
- Night sweats
- Hair loss
- Acne and skin changes
- Dry eyes and loss of collagen
- Vaginal dryness and sensitivity, discomfort during sex, or an increase in urinary tract infections (UTIs)
- Difficulty with sleeping
- Changes in mood
- Brain fog
- Musculoskeletal changes, including joint pain and tendon issues
- Changes in breast composition
Myth: Menopause causes weight gain from fat.
Weight gain isn’t associated with menopause. However, weight from your hip area may be redistributed to your midsection.
Myth: Menopause is causing my (fill in the blank).
Women may misinterpret common midlife symptoms as menopause-related, including:
- Osteoarthritis and other natural wear and tear on the body
- Genetic hair loss (which differs from menopausal hair loss)
- Natural vision and hearing changes — or anxiety and depressive episodes — that occur with aging
- The onset of thyroid, heart, diabetes, and other chronic disorders
While these symptoms are not caused by menopause, they are often worsened by it.
Perimenopause Brings Change
During a woman’s fertile years, hormones such as estrogen, progesterone, luteinizing hormone (LH), and follicle-stimulating hormone (FSH) regulate ovulation, which is the development and release of eggs from the ovaries.
These hormones control the monthly menstruation cycle via complex feedback loops. Their levels rise and fall in relation to one another, regulating and prepping the uterus before ovulation and then shedding the uterine lining after a period.
But as a woman enters perimenopause, the number of eggs decreases, leading to dysfunction and miscommunication in these feedback loops. This results in fluctuating estrogen and progesterone levels, causing the various symptoms of perimenopause and menopause.
Hormone Replacement Therapy Benefits
For many women in perimenopause, hormone levels shift dramatically each month. We study our patients carefully to determine how to “steady the ship.”
One option is hormone replacement therapy (HRT). This treatment helps post-menopausal women restore decreasing levels of estrogen and progesterone.
Properly administered, stable low doses of hormone alleviate uncomfortable symptoms like hot flashes, night sweats, mood swings, sleeplessness, irregular bleeding, and vaginal dryness (and may help prevent osteoporosis, cardiovascular disease, and metabolic disorders).
The prescribing doctor determines the most appropriate form of HRT when working with the patient:
- Oral contraceptive pills (OCPs) consist of estrogen and progesterone or progesterone alone. They help suppress the hormone “chaos” during perimenopause and prevent pregnancy.
- Prescription estrogen via pills, transdermal patches, gels, and creams. Many consider the patch to be an effective HRT method.
- When used alone, estrogen may lead to endometrial cancer in some women, so it’s typically combined with progesterone to stabilize and protect the uterine lining. Progesterone helps promote good sleep.
- Less commonly, a woman may receive testosterone as part of her hormone replacement therapy. Only about 75% of a woman’s testosterone comes from the ovaries, with the rest produced elsewhere in the body, so there are no standardized guidelines for testosterone administration. It’s typically used only in women with premature surgical menopause or very low libido and muscle mass.
Hormone Replacement Therapy Risks
Using HRT during perimenopause or menopause may bring certain risks:
- Estrogen may increase the chance of blood clots, heart attack, stroke, and breast or endometrial cancer — particularly in women who smoke or have a history of one of these conditions — so doctors often avoid its use in patients with these risk factors.
- Progesterone may promote fluid retention and bloating, stress and anxiety, or — in extreme cases — breast cancer.
- Although there’s little long-term data regarding the use of testosterone in menopausal women after two years, we know it encourages mood changes, hirsutism, acne, or weight gain. Testosterone may even be associated with cardiovascular events and certain cancers.
Interesting Facts About Menopause: HRT Was Once Dropped by Doctors
Before the 2000s, post-menopausal women were routinely treated with estrogen and progesterone (HRT), eyeing certain benefits. These included reducing bone loss, decreasing cardiac events, lessening hot flashes, preventing memory loss, and improving the effects of aging on skin and hair, mood, and sleep.
But, a Women’s Health Initiative study in 2001 published surprising signals that HRT might increase a woman’s risk of heart attack and stroke. In an abundance of caution, doctors quickly discontinued the therapy — and for the next two decades, many women experienced unnecessary perimenopausal symptoms.
(During that time, several for-profit hormone clinics sprang up to fill the gap, offering implanted hormone pellets and compounded hormones, with little data or evidence to support their effectiveness.)
More recent research indicates that the risk of cardiovascular events isn’t elevated in women who begin HRT before age 60 or within 10 years of the onset of menopause.
Seek Safe HRT Management and Treatment
Doctors prescribe forms of HRT based on a woman’s symptoms — for example, a combination of hot flashes or night sweats, vaginal changes, and disrupted sleep.
If you seek care for perimenopausal symptoms, consult a well-trained physician in a primary care setting. (A good primary care doctor may also find that a patient’s chronic condition is unrelated to perimenopause.)
Treatments and Settings to Avoid
- While for-profit hormone clinics promise you’ll feel like “Superwoman,” many of these facilities don’t meet the standard of care for appropriate, safe use of hormone therapy.
- Avoid bioidentical hormones (with structures similar to physiologic hormones) prepared by compounding pharmacies. Compounded versions of estrogen or progesterone aren’t FDA-approved, are often unproven, and carry risk. They’re only as good as the pharmacy compounding them.
- Pellets implanted under the skin to deliver doses of hormones carry risks. The pellets can’t be removed and continue to be reabsorbed, even when contraindicated, such as in cases of breast cancer, blood clots, strokes, or heart attacks.
Alternatives to HRT
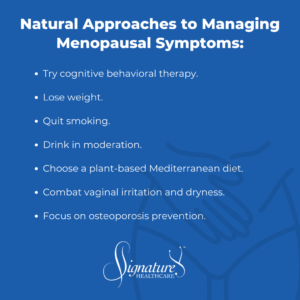
Before you try HRT — or if you prefer an alternative — here are other approaches that may help:
- Try cognitive behavioral therapy. You may better manage menopausal symptoms by reframing challenging thoughts or restructuring your obligations or environment.
- Lose weight. Exercise and weight loss help reduce hot flashes and the risk of chronic diseases associated with midlife.
- Quit smoking. It’s likewise associated with hot flashes and chronic disease.
- Drink in moderation. Alcohol encourages weight gain, spurs hot flashes, and disrupts sleep.
- Choose a plant-based Mediterranean diet, considered one of the healthiest in the world. You’ll reduce weight and improve blood pressure and other critical biomarkers.
- Combat vaginal irritation and dryness. Utilize lubricants, pH adjusters, and topical DHEA supplements for relief.
- Focus on osteoporosis prevention. With your doctor’s advice, take calcium and vitamin D. Participate regularly in weight-bearing and resistance-training exercises.
Interesting Facts About Menopause: Vaginal Issues
Many women are lucky enough to escape significant menopausal symptoms like hot flashes or night sweats — or perhaps they’re past the time when they need HRT.
However, patients may call me with another issue, such as repeated or persistent yeast infections that don’t respond to over-the-counter treatments. Women experience these symptoms during perimenopause, early menopause, or long-term menopause.
Changes in vaginal tissue affect the vagina’s pH level, causing genitourinary syndrome of menopause — irritation, pain with sex, or recurrent UTIs. Treatment with topical estrogen helps heal the affected tissue.
Interesting Facts About Menopause: Vasomotor Issues
We help manage vasomotor symptoms (hot flashes and night sweats) in women who aren’t candidates for estrogen treatment with SSRIs and SNRIs, such as Lexapro, Cymbalta, Gabapentin, or Lyrica.
Estrogen-related modulators are being studied and are currently used selectively for osteoporosis or breast cancer prevention.
Anecdotally, some women report that acupuncture tempers their hot flashes. Some women find relief from night sweats by using products like the Chilipad cooling mattress pad or the Embr smart wristband that delivers a little pulse of cool air. They may also avoid spicy foods or dress in easily removable layers.
There’s not much persuasive data on the use of herbals to control vasomotor issues. We know that large quantities of herbals like soy should be avoided in people with contraindications to estrogen (such as breast cancer or a history of blood clots).
Final Thoughts on HRT and Menopause
Hormone replacement therapy is not a magic bullet against aging, and it’s important to recognize that not every midlife symptom is caused by hormones.
However, HRT can be an invaluable tool for women experiencing real issues in perimenopause or post-menopause.
To learn more interesting facts about menopause, consult reputable sources, such as The New Rules of Menopause and The Menopause Solution by Dr. Stephanie Faubion, president of The Menopause Society.
Or bring your questions to your trusted Signature Healthcare physician. We listen well, look carefully at your symptoms, and work with you on a logical path to relief.
It’s well worth the discussion.

Dr. Elizabeth Abernathy
Dr. Abernathy, board certified in Internal Medicine and a Fellow of the American College of Physicians, has a rich medical background with roots in Charlotte. She graduated from Davidson College, majoring in Medical Ethics, and completed her medical education and a fellowship at UNC Chapel Hill. With 14 years of medical practice in Charlotte, she spent a decade at Carolinas Medical Center teaching ethics, health policy, and clinical decision making. Dr. Abernathy also holds an MHA from UNC Chapel Hill School of Public Health, aiming to enhance her understanding of healthcare systems and economics. Outside of medicine, she enjoys history, travel, literature, and spending time with her family and their foxhound.

