We Diagnose and Treat Patients Faster With Point-of-Care Ultrasound
If you’ve ever had an ultrasound, it may have been a cumbersome process. Perhaps you waited several uncomfortable or anxious days for an appointment at an imaging center. And after your scan, you waited several more days before your doctor had your results to share.
Today, many of my patients don’t need to visit an imaging center to diagnose a problem. With point-of-care ultrasound (POCUS), I can perform an ultrasound right in the exam room. I review the resulting images quickly and effectively — while the patient is with me — and can immediately start any necessary care.
Point-of-care ultrasound eliminates several steps previously involved in ordering a study:
- The ultrasonographer captured the ultrasound image and then sent it to a radiologist.
- The radiologist read the data and returned a diagnostic report to our office.
- Several days after the patient first came to us with a physical complaint, we were finally able to review their ultrasound results and order appropriate treatment.
Versatile Point-of-Care Ultrasound
In an ultrasound scan, sound waves penetrate the body, bounce off soft tissue, and send echoes back to the probe. The echoes convert to electrical signals, and the signal data creates an on-screen image of the probed area.
Ultrasound technology isn’t new. Its use in medicine dates back to 1956. However, the recent boom in ultrasound-on-chip technology makes ultrasound probes more portable and less costly.
Today’s handheld probes fit easily into a doctor’s white coat pocket. They can be used in an exam room or carried to a patient’s bedside without large, costly diagnostic machines.
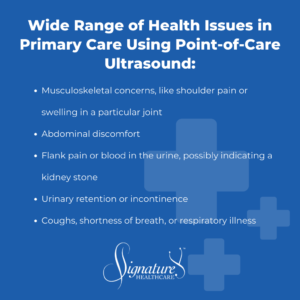
With point-of-care ultrasound, we can test, evaluate, and diagnose a wide range of issues right in the primary care setting, such as:
- Musculoskeletal concerns, like shoulder pain or swelling in a particular joint
- Abdominal discomfort
- Flank pain or blood in the urine, possibly indicating a kidney stone
- Urinary retention or incontinence
- Coughs, shortness of breath, or respiratory illness
We can also use POCUS to track the insertion of needles — perhaps to efficiently retrieve tissue when we biopsy a thyroid disorder or precisely inject nerve blockers to relieve painful fractures or osteoarthritis.
Point-of-care ultrasound can be used to evaluate traumatic eye injuries. Placing a probe over the eyelid might reveal a detached retina, dislocated lens, or inflamed optic nerve. Before, only an ophthalmologist had the equipment to visualize these issues; today, an ultrasound-trained primary care doctor can diagnose them at the point of care.
AI and Wireless Play a Role in Ultrasound
Artificial intelligence (AI) and wireless technologies bring even greater power to portable ultrasound devices.
Traditionally, specialists needed to use ultrasound probes with different-shaped arrays, depending on the contours of the area evaluated. But ultrasound-on-chip lets a single probe accommodate a range of linear, curved, square-faced shapes.
When the probe is directed at tissue, AI quickly determines the body part and type of tissue and automatically adjusts the gain, frequency, and depth of the signal.
Via AI, a physician can command an ultrasound probe by voice. Without touching a screen during a sterile procedure, we can simply tell the probe to freeze an image or take a picture — perhaps to easily measure an area or visualize blood flow through vessels. And we can often do this without an assistant standing by.
Point-of-care ultrasound devices can deliver digital images via wireless signal directly to a cellphone, tablet, or TV.
With AI, on-screen images clearly delineate different tissue planes — skin, muscle, tendon, bone, and nerve — so it’s much easier for a doctor to interpret areas of concern.
Availability of POCUS
Other than a few specialists, most physicians are not traditionally trained to interpret ultrasound images. However, with cost-effective probes being more readily available, training and equipment are becoming standard in medical schools and residencies.
Even so, point-of-care ultrasound is not yet available in most standard healthcare offices, and the problem is time. In traditional healthcare, most doctors manage such a large patient base that they have little time to train in ultrasound technology or to scan patients in the exam room. Hence, they refer patients to imaging centers.
In concierge practice, it’s different. Our smaller patient panel means we have more time to spend with you.
My ultrasound training allows me to use the ultrasound probe and answer questions right at the point of care, bringing you greater convenience, faster treatment, and peace of mind.
POCUS Around the World
Beyond the primary care setting, point-of-care ultrasound can help in remote areas of the world with few medical resources, particularly where patients in need can’t travel many miles to an imaging center.
A small but powerful probe bridges the gap: A clinician needs ultrasound gel and access to electricity or batteries to charge the device. With this simple tool, they can potentially uncover signs of pneumonia or a ruptured lung, evaluate a growing mass, or guide with fluid removal from a patient’s chest or around the heart.
Inexpensive, easy to learn, and portable, it’s inspiring to think about how POCUS technology can contribute to global health.
We’re Here for Your Health
Here in Charlotte, your Signature Healthcare physicians are proud to offer you responsive, personalized healthcare, including point-of-care ultrasound.
Stay in touch with your team!

Dr. Andrés Sánchez
Dr. Sánchez is board-certified in Internal Medicine. Originally from Medellin, Colombia, Dr. Sánchez immigrated to Miami, FL at the age of 11. Dr. Sánchez obtained a Bachelor of Science Degree in Biochemistry from the University of Florida, went on to receive a Dean’s Fellowship to earn his Doctor of Medicine Degree at the University of Rochester School of Medicine, and completed his internal medicine residency at Yale University.
What drives Dr. Sánchez’s way of life, including his practice of medicine, is his Christian faith, which encourages him to exercise grace and compassion in the care of his patients. He enjoys playing the cajón and spending quality time with his wife Cristina, son Caleb, and his church family. Dr. Sánchez makes it a priority to keep up-to-date with medical knowledge and biotechnological advances because he understands how the timely application of these can translate to relieve the suffering of his patients. Dr. Sánchez is fluent in English and Spanish.

