What Is Sleep Fragmentation? How Broken Sleep Affects Us
Suppose you got a good night’s sleep but still wake up tired. Now you’re driving on a busy road or attending an important meeting and can barely keep your eyes open. What’s going on? Is such drowsiness normal?
You may be feeling the effects of sleep fragmentation.
What is sleep fragmentation? It’s another way of saying “broken sleep.”
What Is Sleep Fragmentation?
Fragmentation happens when sleep is repeatedly interrupted in short episodes — for example, by loud snoring, a hot room, a fussy baby, or the aftereffects of a late-evening glass of wine.
If your sleep is regularly fragmented, it could be detrimental to your health, particularly for the 34% of North Carolinians who get insufficient sleep (fewer than seven hours in a 24-hour period).
Fragmented sleep prevents the brain from slipping into crucial, restorative, deep sleep. Prolonged bouts of broken sleep eventually affect mental health, brain function, and immunity and increase the risk of heart disease, type 2 diabetes, and kidney disease.
Sleep Cycles and Stages
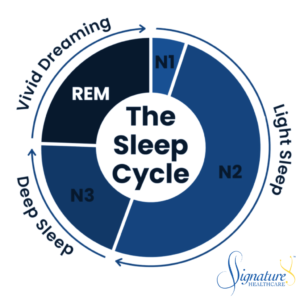
In humans, a normal sleep routine typically includes four to six sleep cycles. Each cycle lasts 90–120 minutes and consists of these stages:
- Stage N1: This is the drowsy pre-sleep phase when your mind and body wind down from the day. Your perception of time dims, and you may nod in and out of sleep.
- Stage N2: You typically spend about half your night’s sleep with your eyes closed in this quiet, restful stage.
- Stage N3: In this slow-wave deep sleep, your body works on physiological repair as it recovers from the day’s exertion and stress.
- Stage NREM: In rapid eye movement (REM) sleep, you enter a state of vivid dreaming. Activity increases in the fluid movement of the brain as it processes the day’s emotions and memories. In the dream state, the body remains immobile, yet the eyes move rapidly while closed.
During N3 and NREM sleep, the brain cleanses itself of the natural buildup of proteins and chemical waste accumulated during the day, resetting and restoring the body for the next day. If you continually awaken before reaching deep sleep or grab only brief periods, you’ll feel fatigued in the morning — sometimes, as if you didn’t sleep.
What Causes Sleep Fragmentation?
Sleep apnea steals sleep. While it’s often considered a benign snoring disease, it’s more insidious than that.
It often goes unrecognized because people don’t remember waking up. They emerge from deep sleep to a lighter sleep phase just long enough for the throat to reopen. This can reset the sleep cycle and delay their return to the beneficial deeper phases.
Besides apnea, here are some other common culprits that can jolt you awake or send you back into lighter, less restful sleep stages:
- Frequent urination, also known as nocturia. Prostate issues in men may cause this.
- Tending to a hungry infant or a child who’s ill or prone to bad dreams.
- Back pain or other chronic discomfort. Chronic pain and fragmented sleep are bidirectional, meaning each can cause the other.
- Sleep disorders, like insomnia, restless leg syndrome, or bruxism (teeth grinding).
- Reflux disease. When the body’s natural mechanisms for clearing acid are impaired, reflux discomfort can awaken the sleeper many times at night.
- Caffeine makes it harder to fall asleep or stay asleep, particularly for people who already have insomnia issues. It may also block the slumberer from entering vital deep sleep.
- Alcohol. Drinking interrupts REM sleep. While it may help you fall asleep, it won’t help you stay there.
- Poor sleep hygiene, including an irregular sleep schedule and other disruptive factors.
- Environmental factors. This includes constant noise, bright light, or uncomfortable temperatures that wake you at night.
- Stress, including anxiety over work the next day.
How Is Sleep Fragmentation Diagnosed?
A patient’s wearable tech, such as a WHOOP device, may provide interesting insights concerning frequently broken sleep. Although the device’s data isn’t sufficient for a medical diagnosis, it may prompt me to dive deeper into the patient’s sleep quality and the factors affecting it.
I may suggest a monitored sleep study, where sleep specialists attach electrodes to a patient’s scalp and examine their EEG while they sleep. Alternatively, in-home sleep testing may be beneficial, particularly when we suspect sleep apnea.
For persistent insomnia, I may also recommend cognitive behavioral therapy for insomnia (CBT-I), a form of sleep training focused on successful sleep hygiene. CBT-I is a great alternative to habit-forming medications.
Essential Sleep Hygiene Tips
If you frequently wake up fatigued, consider these tips to improve your sleep hygiene:
Consistency Is Ideal
- Maintain a consistent sleep schedule. Wake up and go to bed at the same time each day and evening, even on weekends or vacations. Doing so is especially important in your later years when it’s harder to rebound from disturbed sleep. Set a daily routine that makes you tired each night.
- Establish a relaxing bedtime routine. Read a book quietly or listen to a sleep meditation or calming music before bed.
What to Minimize or Avoid
- Limit exposure to bright light in the evenings. Light signals the brain that it’s daytime, preventing melatonin production. Create a sleep-friendly environment in a dark, quiet room.
- Switch bright screens off well before bedtime. I discourage patients from watching the news before bed, as headlines are designed to grab your attention and provoke anxiety that disrupts sleep.
- Avoid caffeine after lunchtime. Consuming caffeine in the afternoon can make it difficult to fall asleep and may prevent your brain from entering deeper sleep phases.
- If you have urinary issues, reduce your fluid intake before bed and fully empty your bladder at bedtime.
- Monitor regular alcohol intake. Often, I see impaired sleep in patients who consume alcohol daily without giving their body a break from it. If you drink right before bedtime, you may wake up once the liver metabolizes those drinks, usually around 2–3 a.m.
- Avoid large meals just before bedtime. If you’re hungry right before bed, eat a small healthy snack, not foods that may give you reflux during the night. Reflux worsens when we lie flat, so consuming a large meal an hour before bed might set you up for a bad night’s sleep.
- Don’t work or watch TV in your bed. Your mind should associate the bed with slumber. Use it only for sleep and intimacy.
Accrue Sleep Debt
- Regular exercise helps you build more sleep debt. For example, I prefer to exercise in the evening so I’m tired and ready for bed at bedtime; if I run in the morning, I often feel like I need a midday nap.
- Retire early enough to get seven or eight hours of sleep, but don’t go to bed until you’re sleepy. Ideally, you want to build up “sleep debt” during the day, so when you head to bed each night, you’re tired and ready to repay that debt.
Manage Time
- Hide the clock in your room, if you can. Doing so may seem counterintuitive, but if you wake in the middle of the night and look at the clock, you’ll be tempted to do the math: “If I fall asleep right now, I can still get five hours of sleep and I’ll be okay tomorrow.” The clock almost taunts you after a while.
- Resist the urge to check the time. Instead, use your internal clock. If you wake up and your alarm hasn’t rung, it’s probably not time to get up. But tossing and turning will make your brain connect your bed with wakefulness.
- If you wake and haven’t fallen back asleep after 10 or 15 minutes (by your own estimation), then get up and do a quiet activity. Avoid looking at bright lights, watching TV, or looking at screens. Consider reading something boring or listening to soothing music until you’re drowsy again.
Let Us Help You Sleep Well
If you still wonder, “What is sleep fragmentation?” or why you frequently wake up and feel tired even after a good night’s sleep, reach out to us.
Your Signature Healthcare doctors can help you discover if you’re getting poor sleep and devise a plan to help your mind and body awaken refreshed. Get in touch and rest easy!

Dr. David Yancey
Dr. Yancey, a board-certified internal medicine specialist, hails from Winston-Salem and holds a psychology degree from Davidson College. He furthered his medical education at The Brody School of Medicine at East Carolina and completed his internal medicine residency at the prestigious Mayo Clinic. Returning to North Carolina in 2010, Dr. Yancey has since been a dedicated hospitalist physician at Carolinas Medical Center in Charlotte. There, he has spearheaded various multi-disciplinary rounding programs and contributed to the training of PA and nurse practitioner fellows.
Outside of his professional pursuits, Dr. Yancey is an avid enthusiast of the great outdoors, enjoying trail running and hiking with his dog. He also relishes traveling, cooking, and assembling jigsaw puzzles with his family.

